The process of deinstitutionalization affected case management by transforming the delivery of mental health services, shifting the focus from institutional to community-based care. This transition presented challenges and opportunities for case managers, requiring them to adapt their practices to meet the needs of individuals living in the community.
Deinstitutionalization led to changes in case management roles and responsibilities, with case managers assuming new skills and knowledge to support individuals in community settings. Case management models evolved to address the unique challenges of deinstitutionalization, resulting in the emergence of various models tailored to different populations and needs.
The Historical Context of Deinstitutionalization
Deinstitutionalization refers to the gradual shift away from institutionalizing individuals with mental illness in large, isolated facilities and towards providing care in community-based settings. This process began in the mid-20th century and was driven by several factors, including the rise of antipsychotic medications, the civil rights movement, and growing concerns about the inhumane conditions in many institutions.
The impact of deinstitutionalization on the mental health care system was profound. As institutions closed, the number of individuals living with mental illness in the community increased significantly. This created a need for new and innovative ways to provide care and support to these individuals.
The Impact of Deinstitutionalization on Case Management Practices, The process of deinstitutionalization affected case management by
Deinstitutionalization presented both challenges and opportunities for case managers. On the one hand, they were now responsible for providing care to a larger and more diverse population of individuals with mental illness. On the other hand, they had the opportunity to develop new and innovative approaches to case management that were more responsive to the needs of individuals living in the community.
One of the biggest challenges that case managers faced was the lack of resources available to support individuals with mental illness in the community. Many of these individuals had difficulty accessing housing, employment, and other essential services. Case managers had to work closely with other agencies and organizations to ensure that these individuals had the support they needed to live independently.
Changes in Case Management Roles and Responsibilities
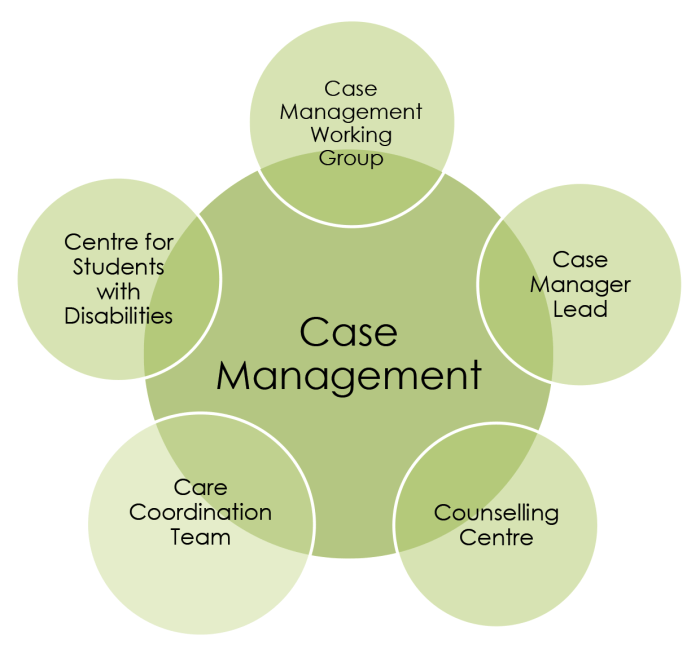
In response to deinstitutionalization, the roles and responsibilities of case managers changed significantly. Case managers became more involved in providing direct services to individuals with mental illness, such as counseling, crisis intervention, and medication management. They also became more responsible for coordinating care between different agencies and organizations.
In addition to these new roles and responsibilities, case managers also needed to acquire new skills and knowledge. They needed to be able to work with individuals with a wide range of mental illnesses, and they needed to be familiar with the resources available in the community.
They also needed to be able to advocate for the rights of individuals with mental illness.
The Evolution of Case Management Models
The challenges of deinstitutionalization led to the development of new case management models. These models were designed to provide more intensive and individualized support to individuals with mental illness living in the community.
One of the most common case management models is the assertive community treatment (ACT) model. ACT teams are composed of a multidisciplinary team of professionals who provide a range of services to individuals with mental illness, including case management, counseling, and medication management.
ACT teams are typically small and work closely with individuals to develop individualized treatment plans.
The Impact of Deinstitutionalization on Service Delivery
Deinstitutionalization also had a significant impact on the delivery of mental health services. Prior to deinstitutionalization, most mental health services were provided in institutions. However, as institutions closed, these services had to be moved to the community.
This shift in service delivery created a number of challenges. One challenge was the lack of funding for community-based mental health services. Another challenge was the difficulty in recruiting and retaining qualified staff to work in community-based settings.
Commonly Asked Questions: The Process Of Deinstitutionalization Affected Case Management By
How did deinstitutionalization affect the roles of case managers?
Deinstitutionalization expanded the roles of case managers, requiring them to develop new skills and knowledge to support individuals in community settings, including providing housing assistance, employment support, and crisis intervention.
What challenges did case managers face during deinstitutionalization?
Case managers faced challenges such as limited resources, lack of training, and stigma associated with mental illness, which made it difficult to provide effective support to individuals in the community.
How did case management models evolve in response to deinstitutionalization?
Case management models evolved to address the challenges of deinstitutionalization, resulting in the development of models such as assertive community treatment, supported employment, and housing first, which focused on providing intensive support and individualized services to individuals with severe mental illness.